Search
- Page Path
- HOME > Search
Original Articles
- Calcium & bone metabolism
Big Data Articles (National Health Insurance Service Database) - Increased Risk of Hip Fracture in Patients with Acromegaly: A Nationwide Cohort Study in Korea
- Jiwon Kim, Namki Hong, Jimi Choi, Ju Hyung Moon, Eui Hyun Kim, Eun Jig Lee, Sin Gon Kim, Cheol Ryong Ku
- Endocrinol Metab. 2023;38(6):690-700. Published online October 30, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1782
- 1,387 View
- 93 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Acromegaly leads to various skeletal complications, and fragility fractures are emerging as a new concern in patients with acromegaly. Therefore, this study investigated the risk of fractures in Korean patients with acromegaly.
Methods
We used the Korean nationwide claims database from 2009 to 2019. A total of 931 patients with acromegaly who had never used an osteoporosis drug before and were treated with surgery alone were selected as study participants, and a 1:29 ratio of 26,999 age- and sex-matched osteoporosis drug-naïve controls without acromegaly were randomly selected from the database.
Results
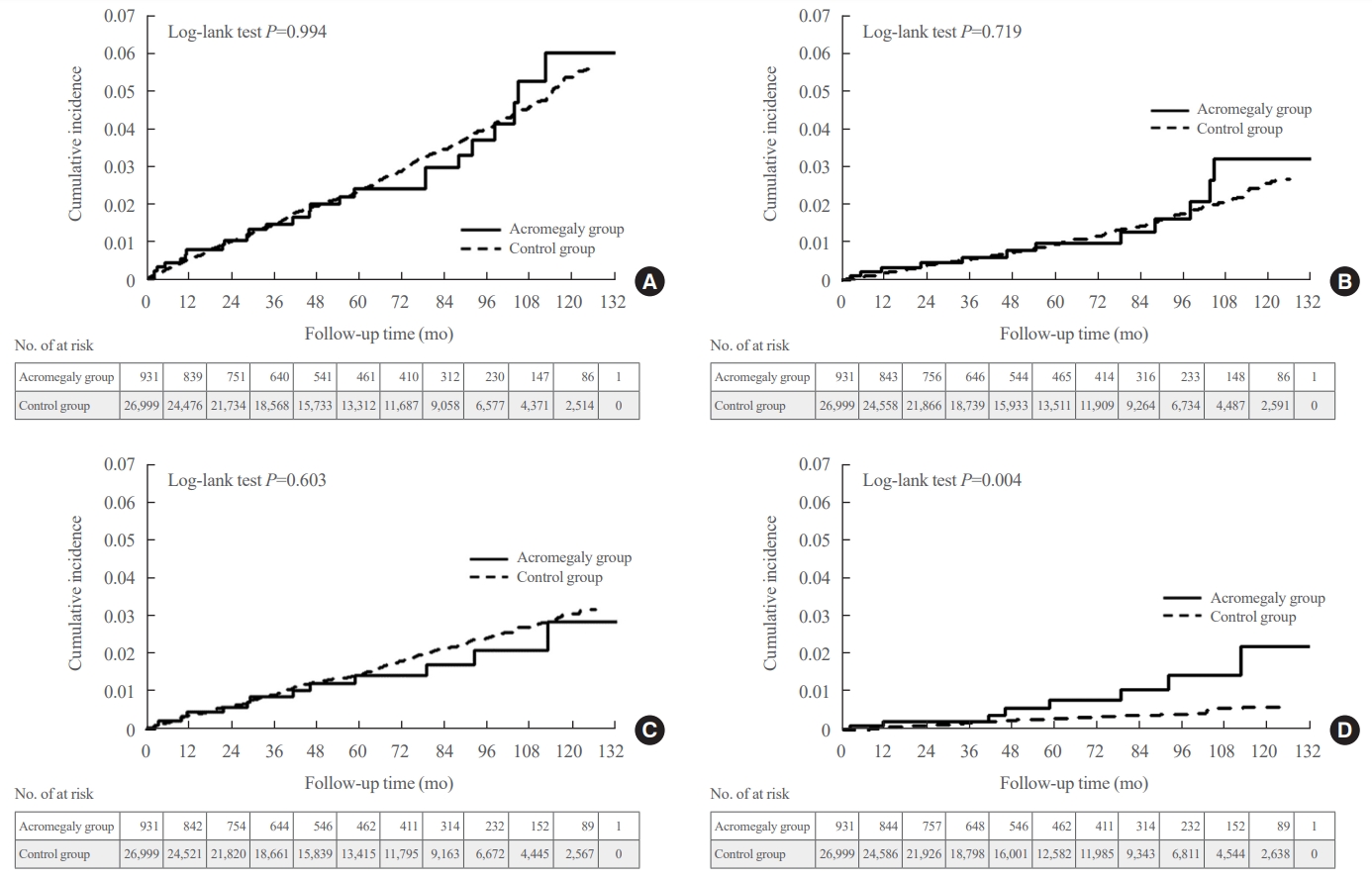
The mean age was 46.2 years, and 50.0% were male. During a median follow-up of 54.1 months, there was no difference in the risks of all, vertebral, and non-vertebral fractures between the acromegaly and control groups. However, hip fracture risk was significantly higher (hazard ratio [HR], 2.73; 95% confidence interval [CI], 1.32 to 5.65), and non-hip and non-vertebral fractures risk was significantly lower (HR, 0.40; 95% CI, 0.17 to 0.98) in patients with acromegaly than in controls; these results remained robust even after adjustment for socioeconomic status and baseline comorbidities. Age, type 2 diabetes mellitus, cardio-cerebrovascular disease, fracture history, recent use of acid-suppressant medication, psychotropic medication, and opioids were risk factors for all fractures in patients with acromegaly (all P<0.05).
Conclusion
Compared with controls, patients surgically treated for acromegaly had a higher risk of hip fractures. The risk factors for fracture in patients with acromegaly were consistent with widely accepted risk factors in the general population.

- Clinical Study
- Associations of GNAS Mutations with Surgical Outcomes in Patients with Growth Hormone-Secreting Pituitary Adenoma
- Hyein Jung, Kyungwon Kim, Daham Kim, Ju Hyung Moon, Eui Hyun Kim, Se Hoon Kim, Cheol Ryong Ku, Eun Jig Lee
- Endocrinol Metab. 2021;36(2):342-350. Published online March 23, 2021
- DOI: https://doi.org/10.3803/EnM.2020.875
- 4,384 View
- 145 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The guanine nucleotide-binding protein, alpha stimulating (GNAS) gene has been associated with growth hormone (GH)-secreting pituitary adenoma. We investigated the prevalence of GNAS mutations in Korean patients with acromegaly and assessed whether mutation status correlated with biochemical or clinical characteristics.
Methods
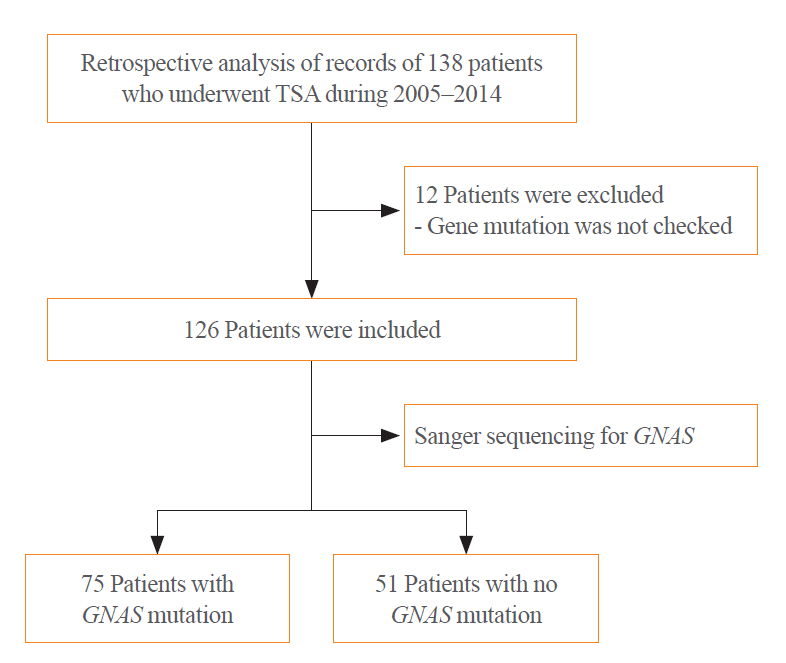
We studied 126 patients with acromegaly who underwent surgery between 2005 and 2014 at Severance Hospital. We performed GNAS gene analysis and evaluated age, sex, hormone levels, postoperative biochemical remission, and immunohistochemical staining results of the tumor.
Results
GNAS mutations were present in 75 patients (59.5%). Patients with and without GNAS mutations showed similar age distribution and Knosp classification. The proportion of female patients was 76.5% and 48.0% in the GNAS-negative and GNAS-mutation groups, respectively (P=0.006). In immunohistochemical staining, the GNAS-mutation group showed higher GH expression in pituitary tumor tissues than the mutation-negative group (98.7% vs. 92.2%, P=0.015). Patients with GNAS mutations had higher preoperative insulin-like growth factor-1 levels (791.3 ng/mL vs. 697.0 ng/mL, P=0.045) and lower immediate postoperative basal (0.9 ng/mL vs. 1.0 ng/mL, P=0.191) and nadir GH levels (0.3 ng/mL vs. 0.6 ng/mL, P=0.012) in oral glucose tolerance tests. Finally, the GNAS-mutation group showed significantly higher surgical remission rates than the mutation-negative group, both at 1 week and 6 months after surgical resection (70.7% vs. 54.9%, P=0.011; 85.3% vs. 82.4%, P=0.007, respectively).
Conclusion
GNAS mutations in GH-secreting pituitary tumors are associated with higher preoperative insulin-like growth factor-1 levels and surgical remission rates and lower immediate postoperative nadir GH levels. Thus, GNAS mutation status can predict surgical responsiveness in patients with acromegaly. -
Citations
Citations to this article as recorded by- Genetic diagnosis in acromegaly and gigantism: From research to clinical practice
Claudia Ramírez-Rentería, Laura C. Hernández-Ramírez
Best Practice & Research Clinical Endocrinology & Metabolism.2024; : 101892. CrossRef - CD8/PD-L1 immunohistochemical reactivity and gene alterations in cutaneous squamous cell carcinoma
Haruto Nishida, Yoshihiko Kondo, Takahiro Kusaba, Kazuhiro Kawamura, Yuzo Oyama, Tsutomu Daa, Avaniyapuram Kannan Murugan
PLOS ONE.2023; 18(2): e0281647. CrossRef - Dynamic monitoring of circulating tumor DNA to analyze genetic characteristics and resistance profile of lorlatinib in ALK positive previously treated NSCLC
Xiya Ma, Kun Zhang, Jing Xu, Hongjun Gao, Shaoxing Yang, Haifeng Qin, Hong Wang, Fang Gao, Xiaoqing Liu
Thoracic Cancer.2023; 14(20): 1980. CrossRef - Multiomics Approach to Acromegaly: Unveiling Translational Insights for Precision Medicine
Kyungwon Kim, Cheol Ryong Ku, Eun Jig Lee
Endocrinology and Metabolism.2023; 38(5): 463. CrossRef - Hotspots of Somatic Genetic Variation in Pituitary Neuroendocrine Tumors
Mariana Torres-Morán, Alexa L. Franco-Álvarez, Rosa G. Rebollar-Vega, Laura C. Hernández-Ramírez
Cancers.2023; 15(23): 5685. CrossRef
- Genetic diagnosis in acromegaly and gigantism: From research to clinical practice

- The One Year Effects of Growth Hormone Replacement on the Body Composition in the Normal Adults.
- Eui Hyun Kim, Suk Chon, Kwan Pyo Koh, Seong Joon Oh, Jeong Taek Woo, Sung Woon Kim, Jin Woo Kim, Young Seol Kim
- J Korean Endocr Soc. 2004;19(4):303-319. Published online August 1, 2004
- 1,026 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The secretion of growth hormone [GH] declines by 14.4% every decade, leading to the suggestion that the elderly are functionally GH deficient, which may increase adipose tissue and decrease the bone mass and density, as well as other negative changes in body composition. Recently, many studies have shown that GH replacement therapy may restore the changes that occur in the body composition with aging. AIM: The GH and insulin like growth factor-I[IGF-I] profiles were identified during GH replacement therapy in the elderly and compared with those of GH deficient[GHD] patients. The metabolic effects of GH replacement on the body composition of the elderly was also investigated, especially the body fat, muscle and bone parameters. Subjects and METHODS: 98 healthy normal out-patients and 13 GHD patients, who had peak GH concentrations less than 5 ng/mL after an insulin tolerance test [ITT] or growth hormone releasing hormone [GHRH] stimulation test, were the subjects of this study. All were receiving appropriate thyroid, adrenal and gonadal hormone replacements. The dose of recombinant human GH [rhGH] was 0.02~0.04 mg [0.06~0.12 IU]/kg of body weight.per week, given nightly by a subcutaneous injection, six times a week, over a 52 week period. The GH was measures after the ITT and GHRH stimulation tests, and the IGF-1, lipid parameters [total cholesterol, triglyceride, HDL-, and LDL cholesterol], visceral adipose tissue [VAT], subcutaneous adipose tissue [SAT], VAT/SAT ratio, quadriceps muscle area, total body fat, total bone mineral density [BMD], alkaline phosphatase [ALP], osteocalcin and urine deoxypyridinoline [DYP], as well as anthropometry, were also assessed. RESULTS: All the anthropometry features between the normal and GHD subjects were very similar. The hormonal profiles were checked; the GH peaks of the ITT and GHRH stimulation tests were significantly higher in the normal compared to the GHD patients, but the GHRH test showed lower GH peaks in than those of the ITT test in the normal subjects. The IGF-I levels after GH replacement were constantly maintained in the normal and GHD groups after 3 week and until the 52nd week. According to the lipid profiles, the GHD group showed significantly decreased total cholesterol and LDL-cholesterol after 12 weeks of GH replacement. The normal male group revealed constantly increased triglyceride levels during the entire 52 weeks of GH replacement, but thr other lipid parameters remained completely unchanged. The normal female group showed no change in any of their lipid parameters. Although the amounts of VAT at the baseline were the same in all groups, only the normal males showed effective visceral fat removal, with significantly reduced VAT after 52 weeks of GH treatment. In the normal female and GHD groups the bone mineral density had a V shaped curve after GH replacement, and the ALP and osteocalcin levels were significantly increased after 26 weeks of GH therapy in the GHD group. CONCLUSION: The body compositions in the normal male, female and GHD groups were similar before the GH replacement therapy, and the serum IGF-I levels were well maintained in all these groups during GH replacement. Although the majority of aging symptoms were improved, the body compositions tended to return to their original stati in the normal groups. GH replacement is recommended in the elderly for better health and well-being

- The Regulation of OPG/OCIF mRNA Epression by IL-1beta in Peripheral Blood Mononuclear Cells.
- In Gul Moon, Ho Yeon Chung, Chang Sun Hwang, Young Soon Kang, Mi Sun Chung, Han Jin Oh, Kyu Hong Choi, Sun Woo Kim, Eui Hyun Kim, Youn Yee Kim, Chang Hoon Yim, Ki VOk Han, Hak Chul Jang, Hyun Koo Yoon, In Kwon Han
- J Korean Endocr Soc. 2000;15(2):204-213. Published online January 1, 2001
- 1,005 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Osteoprotegerin(OPG) is a soluble member of the tumor necrosis factor(TNF) receptor family and inhibits osteoclastogenesis by interrupting the cell-to-cell interaction between osteoblastic/stromal cells and osteoclast progenitors. OPG is expressed in many tissues including osteoblasts and may act on bone tissues in a paracrine and/or autocrine fashion. Futhermore, many cytokines and growth factors are known to influence the regulation of OPG expression in osteoblastic/stromal cells. The aims of the present study were to examine whether or not OPG was expressed in human peripheral blood mononuclear cells(PBMCs) and to investigate the effects of IL-1beta, which were known as potent osteotropic agents, on the regulation of OPG mRNA in PBMCs. METHODS: PBMCs were isolated by centrifugation over Ficoll-Hypaque density gradients from postmenopausal women and cultured in 6-well plates containing alpha-MEM supplemented with 5% FBS. The expression of OPG mRNA in PBMCs was observed by RT-PCR in adherent and nonadherent cells on culture plates. To observe the effect of OPG expression by IL-1beta, we measured the concentration of OPG mRNA by altering the concentration and incubation time of IL-1beta. The measurement of OPG mRNA was done by semi-quantitative PCR and indicated as OPG/GAPDH. RESULTS: OPG was expressed both in cells attached to the surface of culture plates and in non-adherent cells for the incubation of peripheral blood mononuclear cells. The effect of OPG mRNA by IL-1beta tend to increase in accordance with the length of incubation time and maximizes at 12 hours of incubation time and shows 1.2-3.5 times higher than the standard level at the concentration of 0.5ng/ml. However, the increased quantity in concentration varies according to individuals.] CONCLUSION: OPG mRNA is expressed in peripheral blood mononuclear cells and known to be increased by IL-1beta.


 KES
KES

 First
First Prev
Prev



